Thyroid Thursday Episode 60: Hypothyroidism and Fatty Liver
Today we want to talk about the connection between hypothyroidism and something called fatty liver. Fatty liver is a condition where fat is accumulating in the liver. We’re seeing more and more people showing up in the office with fatty liver. I want to talk about how this occurs.
Cellular hypothyroidism which I’ve talked about many times on these Thyroid Thursday videos is decreased T3 in the cells. Thyroid physiology is not about TSH, it’s not about T4, it’s not about what’s necessarily in the bloodstream, but how much T3 is in the cells. Decreased T3 in the cells can cause fatty liver. I want to explain the mechanism. When you have decreased T3 inside your cells, you decrease the metabolism of your cells. You slow metabolism down. That means you can’t burn as much energy, as much fuel.
When you have decreased cell metabolism, the mitochondria, which are like the little engines of the cell, can’t use as much glucose for energy. If the mitochondria can’t burn this glucose (this fuel), we’re putting into the system as efficiently we have glucose backing up in the blood. The increased glucose hangs out in the bloodstream, this is what leads people to develop high blood sugar levels.
Increased glucose causes the pancreas to make more insulin. If the cells can’t use glucose than they resist transport into our cells. The cells start to become resistant to it. Insulin is what carries glucose into the cells and in time, if the cells aren’t using all the glucose, the cells start to resist the glucose and, so we develop this insulin resistance. The pancreas must keep making more and more insulin to force glucose into the tissues. Extra glucose that can’t be used by your liver and muscles is stored as fat. If you’re mitochondria can’t burn glucose, instead of having it buildup in the blood, the body tries to get rid of it, and puts it into fat tissue. You get glucose being stored as fat.
We see insulin resistance start to occur in the liver. It’s one of the first tissues that become insulin resistant. Not all the tissues become insulin resistant at the same rate. If the liver cells start to become insulin resistant, they can’t take in as much glucose and that triggers some mechanisms to occur. Along with the liver starting to become insulin resistant, we start to have this accumulation of fat tissue or what we call adipose tissue. Fat cells increase inflammation in in the body, called systemic inflammation.
Some of the things this inflammation can do is it can increase the conversion of 25OHD (which is inactive vitamin D and what most doctors test) to the active form 1,25HD (which is what most doctors don’t test). When we see increased 1,25OHD, this can be good at times because it can suppress immune system function. Some people might think is a great idea especially those struggling with autoimmune conditions like Hashimoto’s. However, Hashimoto’s and other autoimmune conditions that are driven by what’s called the TH1 system, are often driven by chronic low grade, subclinical infections. If we have these chronic low grade, subclinical infections that are driving the autoimmune attack and we increase 1,25D, we suppress the immune system, so it can’t fight the infection. Short term you may feel a little bit better but long term we just have this chronic progressive infection which continues to drive an autoimmune condition.
The second thing is this inflammation driven from the adipose tissue creates systemic inflammation. Increased systemic insulin resistance starts to ensue because inflammation can help make us insulin resistant. We also see an increase in the Deiodinase 3 activity inside cells. It is the Deiodinase 3 enzyme that converts T4 to reverse T3 instead of active T3. Remember, it’s active T3 inside the cells that stimulates metabolism. If we get more T4 converted to reverse T3 instead of T3, that feeds this mechanism. T3 can also be converted to T2 by this D3 enzyme so overall, we get decreased T3 in the cells which feeds this mechanism. It keeps recycling it. (Slowed cellular metabolism leads to reduced utilization of glucose by the mitochondria and the increased conversion of glucose to fat). We also get decreased insulin secreted over time.
Why would that happen?
The pancreas requires T3 inside the cells to drive and produce insulin. Initially the pancreas is working hard to try and make more insulin and not all cells are affected by cellular hypothyroidism at the same rate or level and so eventually as this process goes on for five or 10 years, the pancreas decreases insulin production. As it decreases insulin production, that can create a host of issues. But, when we’re talking about this mechanism, as we have decreased insulin secretion by the pancreas, with the combination of insulin resistance, especially at the liver, we have our increased dietary glucose being stored as fat (lipogenesis) and we have something happening called increased lipolysis (breakdown of fat).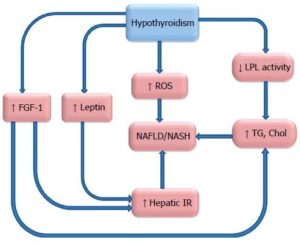
If the liver can’t get sufficient levels of glucose due to the insulin resistance and the lack of insulin being produced by the pancreas, now what happens is the fat stores start to become up regulated to release fat. That’s a process called lipolysis. That fat now gets into the bloodstream as free fatty acids, it’s transported to the liver and the liver tries to convert those free fatty acids into something called acetyl-CoA which can be used by the mitochondria to make energy. If the energy driven from the lipolysis can’t be used because of decreased T3 in cells, the acetyl-CoA winds up getting converted to fat and stored in the liver.
The last piece of this is insulin resistance of the adipose tissue. Eventually all the cells, especially the fat cells, start to become insulin resistant. You see serum glucose levels rise because all the tissues are really struggling to get glucose because of the insulin resistance and the decreased insulin production. In time you get chronic lipolysis. The fat cells are constantly liberating free fatty acids. You’ll see triglyceride levels shoot up on your lab reports. The triglyceride elevation is the result of increased production of triglycerides by liver and excess lipolysis. This all occurs because of decreased T3 in cells. The mitochondria can’t use the Acetyl-Coa liberated from the fat cells effectively and now that extra energy gets stored as fat. The liver just gets fatter and fatter and fatter with all this fat being stored there.
What can you do?
- You’ve got to reduce stress because stress triggers inflammation. Stress creates cellular hypothyroidism.
- You need to improve your sleep quality because when we don’t sleep well we can’t heal and repair well.
- You need to reduce the processed foods in your diet. You need that whole food diet that we talked about. Low carbs, low processed sugars, low processed oils.
- We need to address subclinical infections because many times subclinical infections are at the root of people’s immune, inflammatory and autoimmune issues.
- You need to address any toxicity issues that are present. When the liver gets compromised (fatty liver), it can’t detoxify as well as it could when it was healthy.
You may need the help of a functional medicine practitioner to help you with this process. If you’re told you have fatty liver, there’s probably a thyroid mechanism. Cellular hypothyroidism is likely at the root of the problem. Hopefully this helps. If you need any help with this type of information, you can always call my office or reach out to me via any of the contact information below this video.
Take care.






